Transforming Diabetes Through Real-Time Data: Wearables + CGM
I have worn real-time continuous glucose monitoring (CGM) for over 60,000 hours, offering a truly eye-opening view into my own diabetes and blood sugar trends. With a glucose value on my phone every five minutes, plus data from an activity tracker, I’ve learned a lot: how walking can help dramatically reduce high blood sugar after meals; how too little sleep and too much stress can drive my blood sugar high for hours at a time; and how different foods and diets affect me.
Through these lessons, I have taken steps to improve my A1c by over 1%, increased my time-in-range (70-140 mg/dl) by multiple hours per day, and reduced my daily burden of managing diabetes. I firmly believe the combination of real-time CGM and activity/sleep data can help transform diabetes.
Why will real-time data drive transformation in diabetes?
- Diabetes is a data disease: at least 42 factors influence blood sugar. Data is the most underrated weapon to solving the blood sugar puzzle, since it helps drive profound personal learning, experiments, iteration, and guidance for healthcare providers.
- Glucose, activity, and sleep are huge players in diabetes, but often “invisible.” It’s impossible to manage and understand these variables unless we objectively measure them with easy-to-use devices that fit into everyday life.
- Giving people their own data in real-time is a powerful behavior change tool vs. simply telling people to “do X.” Imagine hearing “You should get 7-9 hours of sleep!” vs. “On days when you get less than 7 hours of sleep, your blood sugars are 20% higher, you are more stressed, and you are less active.” That’s a meaningful difference – personalizing the advice based on one’s own data makes the message far more persuasive. Technology can measure this data now, but the insights often occur in silos. In the future, I believe data from CGM and activity trackers like Fitbit will seamlessly interact, pushing powerful behavior change insights to users.
- Diabetes experiences vary widely from day-to-day and person-to-person. While we tend to focus on averages in healthcare, n=1 personalized care is the goal. CGM and wearables can help us move from “here’s what works on average” to “here’s what works for you” or even “here’s what will work for you today, based on your recent patterns.”
Examples of CGM + Wearable Data Leading to N=1 Personal Learning
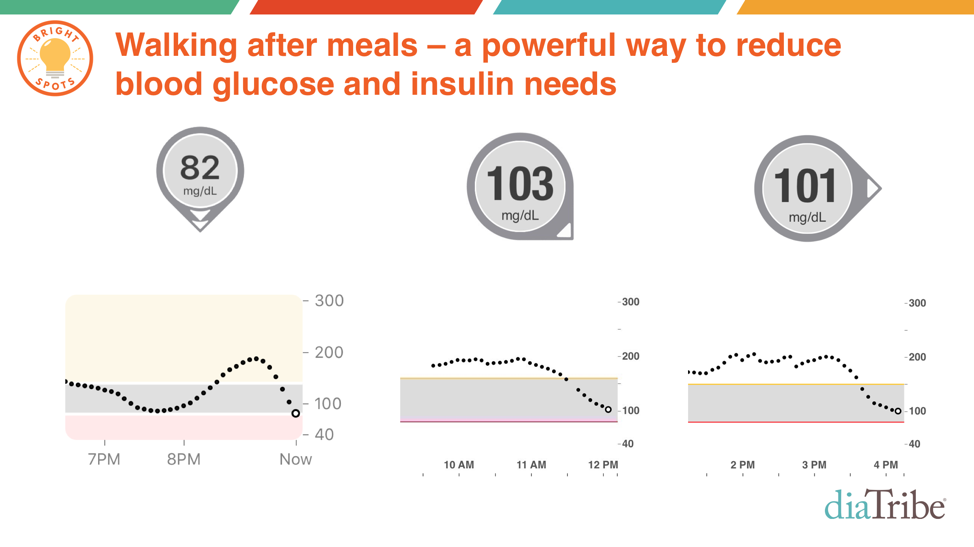
- Walking After Meals: Here are just three example CGM traces – out of several thousand I’ve collected – showing the blood sugar impact of walking. Personally, I’ve found a 20 minute walk can drop my blood sugar by at least 20 mg/dl and sometimes up to 60 mg/dl. Now that’s powerful medicine, especially because walking is free!
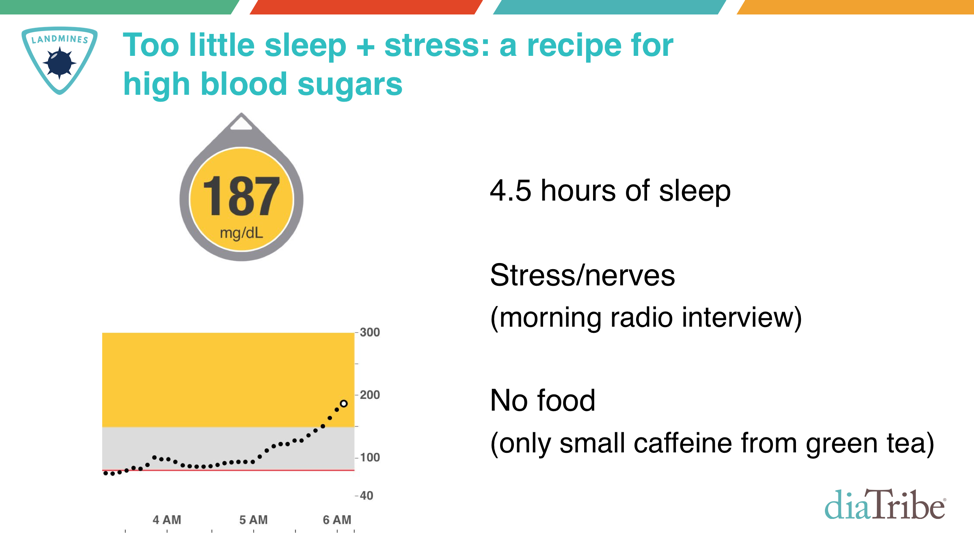
- Stress and Lack of Sleep: Most of the diabetes narrative focuses on food, medication, and exercise, forgetting two equally important variables: stress and sleep. Here’s an example from my own data: 4.5 hours of sleep and stress before a live early morning radio interview. My blood sugar spiked by 90 mg/dl within 45 minutes, without even eating!
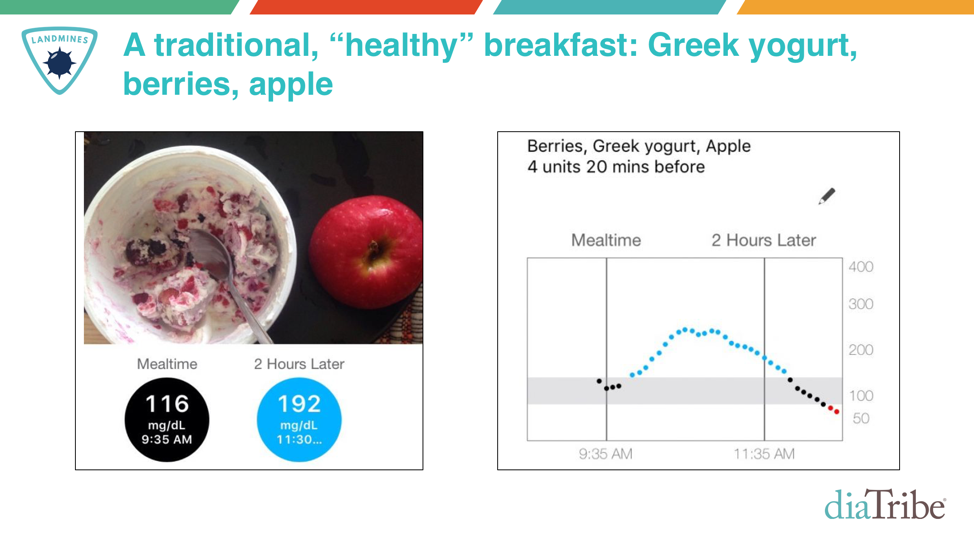
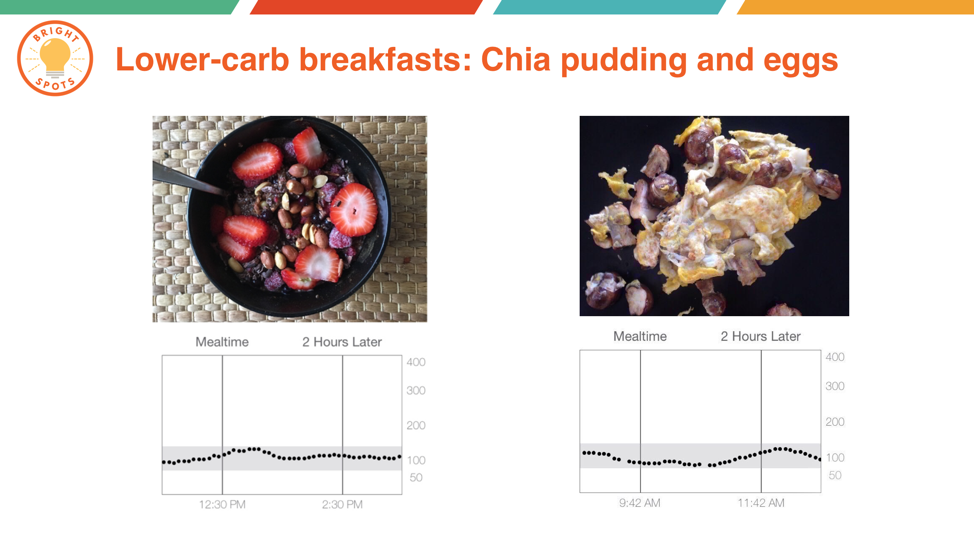
- Impact of Different Foods/Diets: Perhaps the most important thing CGM has taught me is the impact of different foods and diets on my blood sugar. In the slides below, notice the difference in blood sugar from a “healthy” breakfast – unsweetened Greek yogurt, berries, and an apple – relative to my usual lower-carb breakfasts. What’s more, I did everything right for the higher-carb breakfast: I counted every gram of carbohydrate and dosed insulin 20 minutes before the meal. CGM is such a fantastic tool, especially paired with meal photos – I learned very quickly which foods keep my blood sugar in range and which drive it high.
The Importance of “Bright Spots” Framing
I’ve summarized these personal insights in a book, Bright Spots & Landmines: The Diabetes Guide I Wish Someone Had Handed Me. To date, over 90,000 copies have been sold/downloaded, and we’ve received some striking reviews – A1c drops of 2%, impressive weight loss, and dramatic reductions in diabetes burden.
One of the book’s messages that has resonated strongly is the importance of “Bright Spots” framing, especially when it comes to real-time data. We must remind people of when they are doing well and what behaviors enabled that, so those Bright Spots actions can be replicated. Most of what we do in diabetes is the exact opposite: focus on what’s going wrong and how to reduce it (Diabetes Landmines). While Landmines framing can be useful, it can also drive a constant stream of negativity, frustration, shame, and guilt.
Here’s what I mean:
- Landmine framing: “On days when you get less than 7 hours of sleep, your blood sugars are 20% higher, you are more stressed, and you are less active and productive at work. You should get more sleep.”
- Bright Spot framing: “On days when you get more than 7 hours of sleep, your blood sugars are 20% lower, you are more active and productive at work, and you are less stressed. Nice!”
Even those statements share the same insight, notice how much more motivating the second one is? That’s what I hope we can do more of in diabetes by combining CGM data, activity and sleep data from wearables like Fitbit, and smart data science!
Read more from Adam Brown in his diaTribe.org column, Adam’s Corner, and his acclaimed book, Bright Spots & Landmines.



